How Does COVID-19 Compare to Other Pandemics?
Coronavirus disease (COVID-19) is the most recent disease to be declared a pandemic affecting the worldwide population.
Although much of society has grown used to living with COVID-19, it is still a relatively new virus that many people are still trying to understand.
This article will explore how COVID-19 compares to other pandemics in our history.
The first case of COVID-19 was reported on the 1st of December 2019. It is highly infectious and particularly harmful to older adults over the age of 65 years old and immune-compromised individuals.
COVID-19 has symptoms common to those that come with the common flu. They can range from mild to severe. Initial symptoms may include:
In some cases, COVID-19 can lead to more severe health issues such as respiratory complications, heart damage, and death.
There have also been reports of people who contract COVID-19 developing Long COVID. This is where symptoms of the initial infection last longer than the standard 4 weeks of infection.
Researchers have found that COVID-19 is spread through infected airborne droplets that can be inhaled or ingested. These droplets can linger in the air for a few seconds or accumulate on larger surfaces that many people can touch and spread further.
COVID-19 is typically diagnosed through a RAT or PCR test. No medication treats COVID-19 directly however, milder symptoms can be treated with pain medication and rest. For more severe cases, hospitalisation may be required to administer oxygen, intravenous medication, and assisted ventilation.
After the development of the Pfizer vaccine in 2020 for COVID-19, vaccination is the primary prevention method for contracting and preventing severe symptoms of COVID-19. Infected individuals are required to isolate for up to 14 days and social distancing, regular hand washing, and face masks have been utilised to further prevent the spread of the virus.
According to the World Health Organisation, there have currently been 585 million confirmed cases of COVID-19 worldwide. And as of the 12th of August 2022, there have been 6.4 million deaths worldwide caused by COVID-19.
The Australian Department of Health and Aged Care has reported that 9.8 million Australians have tested positive for COVID-19. Of these cases, 12,886 resulted in death.
It is speculated that these statistics could be higher, as people are typically admitted to the hospital or die from the secondary complications caused, such as respiratory or heart failure.
The Spanish Flu is a form of influenza, which was first reported in 1918 and said to last up until 1920. It was found to have an avian origin and was caused by the H1N1 virus mutating the virus. This was a new form of Influenza A that spread easily and was particularly dangerous for children under 5 years old and older adults over the age of 65 years old.
The Spanish flu had symptoms that were very similar to COVID-19, both in the mild and more severe symptoms. Initial symptoms included:
As the virus worsened, it would affect the respiratory system leading to the development of pneumonia and other respiratory complications. Because many people died from the secondary conditions, many deaths caused by the Spanish flu were not accurately reported.
Spanish flu was similar to COVID-19 in that it was highly infectious. It was transmitted between people through inhaling infected airborne respiratory droplets. As this was a new strain of influenza, most populations did not have a developed immunity to combat it.
Due to the time, there were no effective medications or antibiotics to treat the Spanish flu and its complications. This is said to be one of the reasons that the infection and death rates were as high as they were.
Between 1918 and 1919, a vaccine was produced to prevent death for those who were infected. This vaccine would combat the bacterial infections that came from the secondary conditions as researchers were unable to determine what caused this strain of influenza.
For countries that had time to prepare, the first line of defence was quarantine to try and prevent the virus from reaching the country’s population. Within communities, prevention measures included:
It is estimated that the Spanish flu infected approximately 500 million people worldwide between 1918 and 1919. At the time, this would equal up to 33% of the worldwide population. In addition to this, the Spanish Flu killed 25 million people globally but could be as high as 40-50 million when accounting for deaths caused by secondary conditions such as pneumonia.
Australia was one of the few countries that had time to prepare for the spread of the Spanish Flu and was able to quarantine cases until the virulence lessened. According to the National Museum Australia, approximately 40% of the Australian population contracted the Spanish Flu and of these people, around 15,000 died.
It can be seen from these statistics that the Spanish Flu had a far more detrimental effect on the worldwide population in a shorter time than COVID-19 has thus far. This can be attributed to the advances in medicine and technology as well as implementing procedures learned from previous pandemics, such as the Spanish Flu.
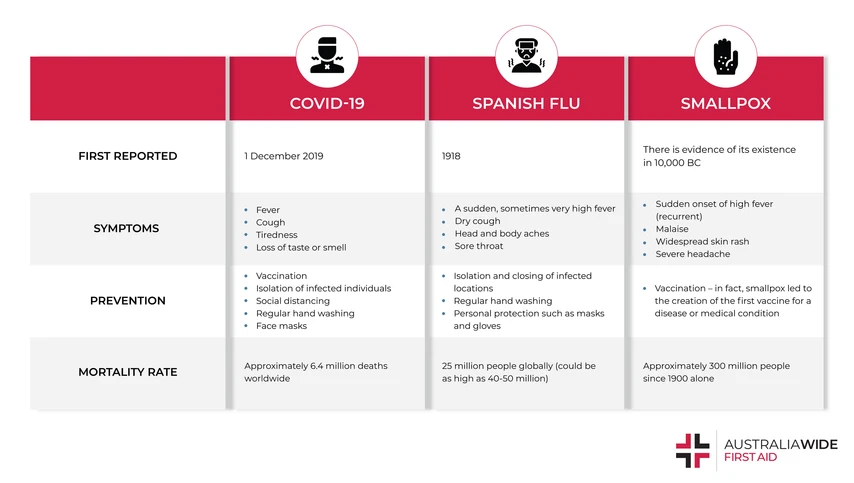
Smallpox was an extremely contagious disease that killed millions of people and lead to the decline of many civilisations. It was caused by infection from the variola virus, an orthopoxvirus. The origin of Smallpox is unknown however, there is evidence of its existence 3000 years ago, seen by the scarring on Egyptian mummies' bodies. In 1977, the World Health Organisation created a worldwide initiative to administer immunisations and Smallpox has since been declared eradicated from this campaign.
The defining symptom of Smallpox was a red rash on the face and body that would develop into small blisters and result in scarring. The accompanying symptoms were similar to those of COVID-19:
Smallpox had a high likelihood of resulting in death, as the virus would attack the bone marrow, respiratory or circulatory systems.
Smallpox had a similar transmission method to COVID-19, in that it spread through interpersonal contact, primarily from inhaling infected airborne droplets. It was also possible for someone to contract smallpox from contact with contaminated objects such as clothing and bedding.
Much like the other pandemics described, there were no medical treatments to treat smallpox directly. Medical treatments administered would be to manage the symptoms of the secondary conditions developed as a result of smallpox.
Smallpox is significant in medical history as it led to the creation of the first vaccine for a disease or medical condition. In 1967, the World Health Organisation developed a plan to create widespread immunity through immunisations, and Smallpox was officially declared eradicated in 1977.
It is difficult to determine accurate statistics for infection and death rate of Smallpox as this disease existed before medical records were kept. However, it is estimated that since the 1900s, 12 million people every year would contract Smallpox and of these cases, approximately 2 million would lead to death.
Based on these statistics, Smallpox appears to have a slightly less significant transmission and death rate than COVID-19. However, it is important to recognise that in the centuries before this when medicine was still being developed, these rates would have been significantly higher.
Although COVID-19 is the first pandemic to affect modern society, it is not the first in our history and certainly won’t be the last. The impacts of COVID-19 have been devastating for many and we are still living in a society that has to manage high infection rates.
Compared to other pandemics, COVID-19 does not appear to be more harmful, and advancements in medicine and technology will help reduce this risk even further.
If you’re interested in learning how to identify, prevent, and treat a variety of health conditions, click here for more information about our First Aid courses.

February 10, 2023
Home to some of the world's most dangerous shark species, Australia is one of the deadliest countries when it comes to human/shark incidents. In this article, we explore the number and outcome of shark/human incidents that occurred in Australia in 2022, to date.

December 20, 2022
Five diseases accounted for more than one-third of all deaths registered in Australia in 2021. And though our overall mortality rate remains low, Dementia is narrowing the gap to become one of Australia's deadliest diseases.

October 24, 2022
Health statistics are an invaluable tool for measuring the health of Australians and targeting prevention and treatment resources accordingly. In this article, we compare Australia's mortality rating from 2019 to 2020.